Diabetes Management
Keeping an Eye on Diabetic Retinopathy
4 min read
By Apollo 24/7, Published on - 02 December 2020, Updated on - 26 January 2026
Share this article
0
14 likes

Causes and stages of diabetic retinopathy
jasjdk djads kjakds akd
Background retinopathy: In this early stage of diabetic retinopathy, the walls of the blood vessels in the retina weaken. It causes tiny bulges called micro-aneurysms that can leak small amounts of blood into the retina. This condition is common in people with diabetes where their vision is not affected but indicates a high risk of developing vision problems in the future.
Pre-proliferative diabetic retinopathy: This is the second stage that occurs when the damaged blood vessels swell, causing fluid and blood leakage into the retina. Sometimes, the macula, the center of the retina responsible for sharp and straight-ahead vision, can be affected. The swelling and thickening of the macula are known as macular edema. This stage usually causes distorted vision.
Proliferative diabetic retinopathy: This stage occurs when the damaged blood vessels completely block the blood supply. It is characterized by abnormal growth and the development of new blood vessels. These new blood vessels are weak and bleed easily into the vitreous (vitreous is the gel-like fluid that fills the center of the eyes). This condition causes vision loss that may be severe.
Symptoms of diabetic retinopathy
Eye floaters (transparent spots or dark strings that float in the person’s vision)
Blurred or patchy vision
Fluctuating vision
Impaired colour vision
Dark or empty spots in the centre of the vision
Sudden loss of vision
Importance of screening
People with type 2 diabetes have retinopathy in the early stages when they get their diabetes diagnosed. For these people, an annual dilated eye examination is recommended shortly after diabetes is diagnosed.
People with type 1 diabetes are advised for annual eye examinations after 3-5 years of diagnosing diabetes.
Preventive steps
Managing diabetes: One should follow a healthy diet and be physically active. It is recommended that people with diabetes exercise or walk for at least 150 minutes a week. In addition to this, they must take oral diabetes medications or insulin as prescribed by the doctor, and not miss any doses.
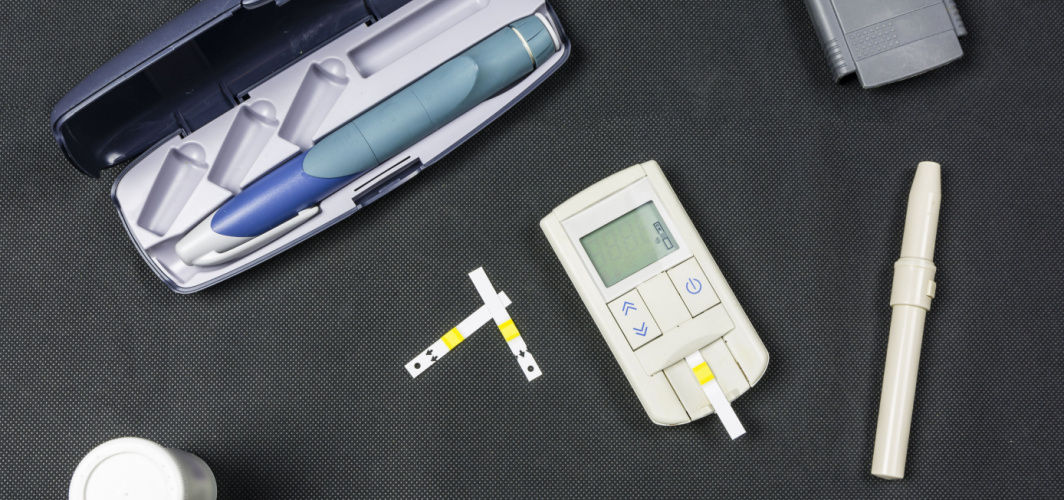
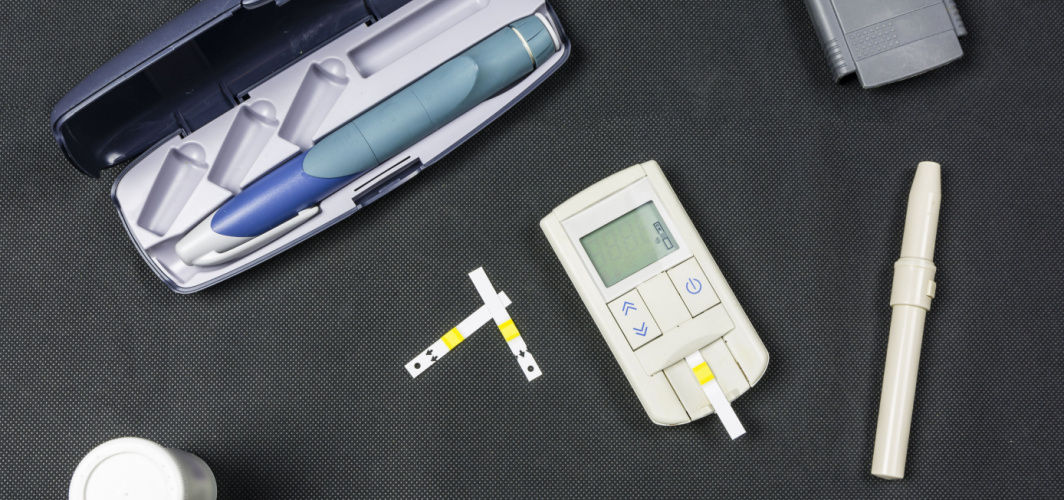
Monitoring the blood sugar level: People with diabetes must check and record their blood sugar levels frequently. This will help to take measures to keep sugar levels in a healthy range.
Testing for HbA1c level: HbA1c test reflects the average blood sugar levels for the last 3 months. One should aim to keep the HbA1c under 7 percent.
Keeping blood pressure and cholesterol under control: Healthy diet, regular exercise, and a healthy weight help keep these levels under check. However, sometimes medication may also be required.
Quitting smoking: Smoking may increase the risk of developing various diabetes-related complications. Quitting smoking will help to reduce the risk of diabetic retinopathy.
Being mindful of vision changes: Any changes in vision such as floaters, dark spots, or blurred vision should be immediately discussed with an eye specialist.
Conclusion
JavaScript Alert
Diabetes Management
Consult Top Diabetologists
View AllLeave Comment
Recommended for you

Diabetes Management
To Avoid Health Complications, This Is How Frequently You Should Check Your Blood Glucose
Tracking blood glucose levels is vital for diabetes management. The article explains how many times you need to check fasting and postprandial blood glucose levels.
Diabetes Management
What Do Diabetes Test Packages Include?
A glucose random test is a simple procedure that requires no overnight fasting or any special preparations. It simply involves pricking the finger to obtain a drop of blood, which is placed on a test strip of a glucometer for blood glucose reading. A sugar level of 140 mg/dL or below is generally considered normal. This test provides a quick assessment of blood sugar levels without the need for fasting or specific timing.

Diabetes Management
Hypoglycaemia: Know What Happens When Your Blood Sugar Drops!
Hypoglycaemia is common in diabetics but can occur in healthy people too. Recognizing the symptoms is important to avoid complications. Treating the underlying cause and making dietary changes can help in preventing hypoglycaemia.
Subscribe
Sign up for our free Health Library Daily Newsletter
Get doctor-approved health tips, news, and more.
Visual Stories

8 Fruits That are Incredibly Healthy for Diabetes
Tap to continue exploring
Recommended for you

Diabetes Management
To Avoid Health Complications, This Is How Frequently You Should Check Your Blood Glucose
Tracking blood glucose levels is vital for diabetes management. The article explains how many times you need to check fasting and postprandial blood glucose levels.
Diabetes Management
What Do Diabetes Test Packages Include?
A glucose random test is a simple procedure that requires no overnight fasting or any special preparations. It simply involves pricking the finger to obtain a drop of blood, which is placed on a test strip of a glucometer for blood glucose reading. A sugar level of 140 mg/dL or below is generally considered normal. This test provides a quick assessment of blood sugar levels without the need for fasting or specific timing.

Diabetes Management
Hypoglycaemia: Know What Happens When Your Blood Sugar Drops!
Hypoglycaemia is common in diabetics but can occur in healthy people too. Recognizing the symptoms is important to avoid complications. Treating the underlying cause and making dietary changes can help in preventing hypoglycaemia.