Diabetes Management
Prevention Tips For Diabetes Foot Infection
4 min read
By Apollo 24|7, Published on - 28 November 2022, Updated on - 05 September 2023
Share this article
0
1 like
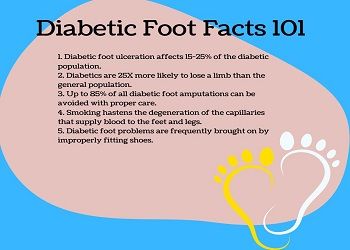
It is rather alarming to learn that a limb is amputated every 30 seconds on average due to a diabetic foot infection. According to a study, patients with diabetes account for 40 to 60 percent of all lower limb amputations.
More than 85% of these amputations are caused by foot ulcers that progress to gangrene or severe infection. An estimated 3-8% of people have diabetic foot ulcers. To prevent such complications, aggressive management and education of the patients and caregivers are of utmost importance.
In this blog, we will discuss the predisposing risk factors for foot infection in patients with diabetes and measures to prevent its complications.
What Causes Diabetic Foot Ulcers?
Let's start with the basics and figure out what happens to the body in diabetes. When blood sugar levels are out of control, it can cause damage to the blood vessels and the nerves, resulting in poor blood circulation. Inadequate blood supply to the foot increases the chances of foot ulcers in case of foot care neglect.
These ulcers either never heal or take an exceptionally long time to heal, leading to the inevitable onset of an infection. Infections of the soft tissue or bone below is referred to as diabetic foot ulcer. These typically necessitate hospitalization and may even lead to limp amputation.
Damage to blood vessels is a direct result of uncontrolled diabetes. When blood sugar levels are consistently high, they cause damage to the blood vessels in the foot, which reduces blood flow. In the absence of treatment, the affected areas (often the feet) become numb, painful, and lose their sense of feeling.
Did You Know?
Approximately 15% of people with diabetes develop foot ulcers, which are open sores or wounds, most often on the soles of their feet.
What Are the Common Signs of Diabetic Foot?
In the event that you have diabetes, you should always be on the lookout for signs such as
- Leg cramps
- Swelling
- Burning sensation
- Itching
- Skin discolouration
- Redness
- Sharp pain
In case, you develop a diabetic foot infection, chances are you will also develop the following:
- Sepsis: Is bloodstream infection which damages tissues and organs. The common symptom is the skin turning blue.
- Gangrene: It's caused due to a lack of blood flow or a bacterial infection.
- Skin Infections: Diabetic foot ulcers can develop skin infections, causing swelling, foul-smelling discharge, fever, and chills.
- Abscess Formation: It is the formation of painful pus under the surface of the skin
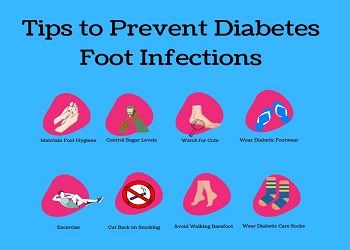
7 Tips To Prevent Diabetic Foot Infection
Yes, diabetics can prevent diabetic neuropathy (diabetic foot infection) with some lifestyle changes like
1. Maintain Proper Foot Hygiene
Wash them every day with a bar of mild soap and warm water.
2. Control Blood Sugar Levels
Make sure your blood sugar level is under control by taking care of your dietary intake.
3. Check Your Feet
Regularly check your feet for new cuts, scrapes, or wounds.
4. Wear Diabetic Footwear
Wear comfortable shoes that fit well and keep your feet safe. And as always, never walk barefoot.
5. Stay Active
Ensure good blood flow to the feet by walking or running every day.
6. Stop Smoking
Cut down on habits like smoking which acts as contributing factor to restricting blood circulation.
7. Watch Out for Ulcers
Do not take care of foot ulcers by yourself! See your diabetologist or a podiatrist right away.
Did You Know?
75% of foot ulcers are preventable!
When Is the Foot Amputated?
Many patients who have diabetes also have peripheral artery disease (PAD), which restricts blood flow to the feet. PAD and diabetic neuropathy, when combined, make it much easier to develop ulcers and infections in the foot.
With time, the risk of foot infection spreading throughout the bloodstream increases. In such a scenario, amputating the damaged foot might be the only way to prevent this from taking place.
Did You Know?
Diabetic foot ulcers and amputations are 2X as lethal for men as they are for women.
Is There a Way to Diagnose Diabetic Neuropathy?
There are several diagnostic tests that can evaluate a diabetic foot:
- X-Ray
It can give doctors a complete picture of the skeletal structure of the foot.
- Ultrasound or Magnetic Resonance Imaging (MRI)
Provides an apparent view of the foot's soft tissues.
- Filament Tests
It is the most accurate way to gauge how sensitive a person's feet are to touch.
- Nerve Condition Tests
The test evaluates how well electrical signals can be transmitted through the lower extremities.
- Electromyography (EMG) Tests
It analyzes electrically the impulses sent out by the foot's muscles.
Final Note
Making simple modifications to your lifestyle can bring noticeable differences to your quality of life. With a clear picture of how an increase in blood sugar levels can complicate foot infections, you are sure to book a diagnostic test right away.
Get in touch with our diabetologists if you want to know more.
You can also manage your diabetes like a pro with Apollo 24|7's 12-week empower programme.
Medically Reviewed by Dr. Dhanunjay Reddy B
Diabetes Management
Leave Comment
Recommended for you

Diabetes Management
What Is Insulin? Answering The Top 5 Frequently Asked Questions
The different types of insulin available for diabetes management are rapid-acting insulin which works quickly and short-acting insulin which is taken before meals to control blood sugar levels. Intermediate-acting insulin has a prolonged effect and is taken twice a day for basal insulin coverage during fasting periods while long-acting insulin provides a steady release of basal insulin for 24 hours to maintain stable blood sugar levels, and pre-mixed insulin that combines short-acting and intermediate-acting insulin.

Diabetes Management
To Avoid Health Complications, This Is How Frequently You Should Check Your Blood Glucose
Tracking blood glucose levels is vital for diabetes management. The article explains how many times you need to check fasting and postprandial blood glucose levels.

Diabetes Management
Aerobic or Resistance Exercises: Which One is Ideal to Manage Blood Sugar?
The American Diabetes Association recommends a combination of aerobic exercises like brisk walking or cycling (at least 150 minutes per week) and resistance training like weightlifting (2-3 sessions per week) for people with diabetes. Aerobic exercises help lower blood sugar by using glucose for energy and improving insulin sensitivity, while resistance exercises improve muscle strength and promote glucose uptake, aiding in blood sugar control.
Subscribe
Sign up for our free Health Library Daily Newsletter
Get doctor-approved health tips, news, and more.
Visual Stories

8 Fruits That are Incredibly Healthy for Diabetes
Tap to continue exploring
Recommended for you

Diabetes Management
What Is Insulin? Answering The Top 5 Frequently Asked Questions
The different types of insulin available for diabetes management are rapid-acting insulin which works quickly and short-acting insulin which is taken before meals to control blood sugar levels. Intermediate-acting insulin has a prolonged effect and is taken twice a day for basal insulin coverage during fasting periods while long-acting insulin provides a steady release of basal insulin for 24 hours to maintain stable blood sugar levels, and pre-mixed insulin that combines short-acting and intermediate-acting insulin.

Diabetes Management
To Avoid Health Complications, This Is How Frequently You Should Check Your Blood Glucose
Tracking blood glucose levels is vital for diabetes management. The article explains how many times you need to check fasting and postprandial blood glucose levels.

Diabetes Management
Aerobic or Resistance Exercises: Which One is Ideal to Manage Blood Sugar?
The American Diabetes Association recommends a combination of aerobic exercises like brisk walking or cycling (at least 150 minutes per week) and resistance training like weightlifting (2-3 sessions per week) for people with diabetes. Aerobic exercises help lower blood sugar by using glucose for energy and improving insulin sensitivity, while resistance exercises improve muscle strength and promote glucose uptake, aiding in blood sugar control.