Diabetes Management
Why is Controlling Diabetes Even More Important During the COVID-19 Pandemic?
6 min read
By Apollo 24/7, Published on - 01 October 2020, Updated on - 01 June 2023
Share this article
0
5 likes

How does COVID-19 impact people with pre-existing diabetes?
- According to the published study in the New England Journal of Medicine, Coronavirus binds to angiotensin-converting enzyme 2 (ACE-2) receptors for entering the human body. The ACE-2 receptors are abundant in the beta cells of the pancreas. These cells control the release of insulin. When the Coronavirus infects these cells, they lose their insulin-secreting capacity with stress and inflammation (due to cytokine storm). This leads to rapid metabolic deterioration with the development of diabetic ketoacidosis.
- People with diabetes have a low immune response and high inflammation compared to persons who have normal blood glucose. Hence, they have a low ability to fight the Coronavirus thereby prolonging the recovery period. Scientific evidence suggests that diabetic people infected by COVID-19 had significantly increased levels of inflammatory markers (cytokines, interleukin-6, tumor necrosis factor, and C-reactive protein). Additionally, Coronavirus triggers the immune response producing T cells and B cells (antibodies). Triggered immune response and inflammation may also lead to ‘cytokine storm’ causing more cell damage in diabetic people than those without diabetes.
Increased risk of diabetes ketoacidosis (DKA)
Clinical evidence correlating higher risk of severe COVID-19 illness in diabetic patients
- The CORONADO study: This is the first study that highlighted the risk of severe COVID-19 illness among people with diabetes (average age 70) admitted to 53 French hospitals between 10- 31 March 2020. Out of a total of 1,317 COVID-19 patients under study, 1,172 (89%) subjects had type 2 diabetes while 39 (3%) had type 1 diabetes. The results reveal that 10% of this group of patients died within 7 days of hospital admission while 20% required ventilator and ICU assistance.
- USA study: In 1,122 patients with COVID-19 admitted to hospitals in the USA, it was found that the mortality rate was four times higher in those with diabetes or elevated blood sugar (hyperglycaemia) during the hospital stay (28·8%) than those with normal blood sugar (6·2%). Moreover, mortality was higher in those with hyperglycaemia and without known diabetes than in patients with known diabetes.
How can people with diabetes stay healthy during COVID-19?
- Take precautions to prevent diabetic ketoacidosis (DKA): COVID-19 can increase the risk of DKA if not controlled and monitored. Signs of DKA include nausea, vomiting, frequent urination, and abdominal pain. So, if your blood glucose level is greater than 240 mg dL in consecutive readings, seeking a doctor consultation to check for ketones is recommended.
- Stock up medications: Try to keep a monthly stock of insulin and anti-diabetic medications as it is risky to go out in public places frequently. Make sure your insulin vials/pens are stored as recommended. Additionally, speak with your doctor to check if you need to keep any medicines handy like paracetamol, antacids, pain relievers, and medications for nausea, diarrhoea, vomiting, etc. to avoid further complications.
- Regular monitoring of blood sugar level: Rapid and high fluctuations in blood sugar levels in a diabetes patient can be serious. Hence, regular monitoring of blood sugar levels is of utmost importance. Diabetes patients should have a glucose monitoring device (glucometer) at home to keep a record of their blood glucose levels.
- Regular physical activity: Besides a healthy diet and medications, physical activity is equally important in the management of diabetes. At least 150 min of physical activity every week is recommended. This can be split into - 15 min of post-meal walking and light exercise for 30 min every day. Consult your doctor before starting a new regimen.
- Follow COVID-19 safety guidelines: You should strictly adhere to the social distancing guidelines, wear a face mask every time you step out, and follow hand hygiene to lower the risk of getting infected.
- Virtual doctor consultation: It may be a better idea to speak with your doctor if you notice any unusual symptoms, or unfamiliar patterns in your blood glucose values. You can opt for an online doctor consultation if you need to discuss your health with your endocrinologist.
You can also manage your diabetes like a pro with Apollo 24|7's 12-week empower programme.
Diabetes Management
Leave Comment
Recommended for you

Diabetes Management
Insulin Therapy for Diabetes: Separating Myths from Facts
Insulin treatment may not lead to weight gain. In type 2 diabetics, undergoing insulin treatment, weight gain is frequently caused by the improved blood glucose control and higher effectiveness in utilising glucose. Insulin itself does not directly cause it. The initial weight increase frequently stabilises with time, proper diet and exercising.
Diabetes Management
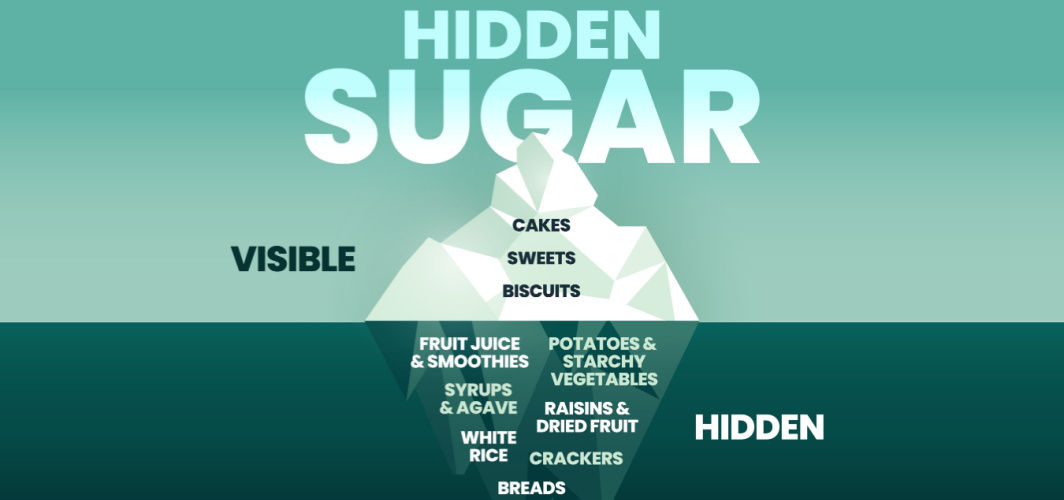
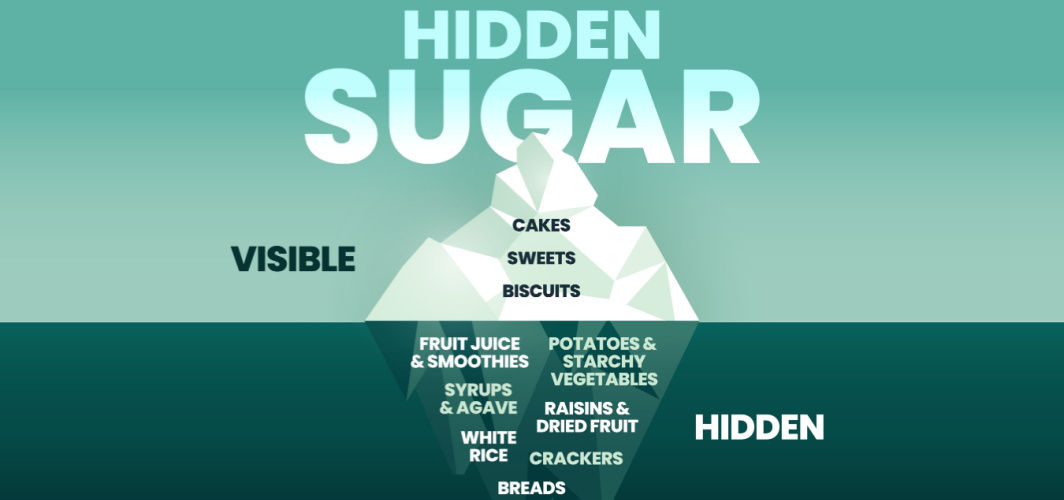
Avoid or Limit These Common Foods with Hidden Sugar
Some foods that may contain hidden sugars include flavoured yoghurt, granola bars, canned fruit in syrup, condiments like ketchup and barbecue sauce, flavoured coffee drinks, packaged sauces and dressings, certain breakfast cereals, and processed snacks. Diabetics should read the food labels and be extra cautious about ingredients to manage diabetes well.

Diabetes Management
Monsoon Care for Diabetes: 9 Things Every Diabetic Must Know
The rainy season can affect people with diabetes as during this time of the year, intestinal & functions become weak which can result in low metabolism and increased fat storage. To stay on track, monitor your levels regularly. Keep insulin and diabetes supplies on hand. Drink clean water to prevent infections, and be cautious with street food. Protect your feet from fungal infections by keeping them dry.
Subscribe
Sign up for our free Health Library Daily Newsletter
Get doctor-approved health tips, news, and more.
Visual Stories

8 Fruits That are Incredibly Healthy for Diabetes
Tap to continue exploring
Recommended for you

Diabetes Management
Insulin Therapy for Diabetes: Separating Myths from Facts
Insulin treatment may not lead to weight gain. In type 2 diabetics, undergoing insulin treatment, weight gain is frequently caused by the improved blood glucose control and higher effectiveness in utilising glucose. Insulin itself does not directly cause it. The initial weight increase frequently stabilises with time, proper diet and exercising.
Diabetes Management
Avoid or Limit These Common Foods with Hidden Sugar
Some foods that may contain hidden sugars include flavoured yoghurt, granola bars, canned fruit in syrup, condiments like ketchup and barbecue sauce, flavoured coffee drinks, packaged sauces and dressings, certain breakfast cereals, and processed snacks. Diabetics should read the food labels and be extra cautious about ingredients to manage diabetes well.

Diabetes Management
Monsoon Care for Diabetes: 9 Things Every Diabetic Must Know
The rainy season can affect people with diabetes as during this time of the year, intestinal & functions become weak which can result in low metabolism and increased fat storage. To stay on track, monitor your levels regularly. Keep insulin and diabetes supplies on hand. Drink clean water to prevent infections, and be cautious with street food. Protect your feet from fungal infections by keeping them dry.